The Value of a Well-Trained Medical Chaperone
The Value of a Well-Trained Medical Chaperone
For some time now, the medical establishment in the U.S. has advocated the use of medical chaperones. The American Medical Association urges physicians to make chaperones available to all patients. Virtually all other medical professional organizations make the same recommendation, especially when it comes to intimate exams. Several states have laws requiring that chaperones be provided during such exams.
Chaperones play an important role during probationary periods.
Recently, some experts in the U.S. generalized from the important concerns raised by an Australian report on the use of chaperones. The 88-page report, titled “Independent review of the use of chaperones to protect patients in Australia” (2017), was comprehensive, but investigated a narrow question. As the author, Professor Ron Paterson, explains at the outset, the purpose of the review was to consider the mandated use of chaperones “to protect patients while allegations of sexual misconduct are investigated” (italics ours). The report concluded that in such situations a chaperone did not provide patients with adequate protection, but then set forth situations and conditions in which chaperones could be useful and appropriate.
PBI Education Medical Director Catherine Caldicott, MD, FACP, says that authorities in this country rarely if ever follow the practice of mandating chaperones during investigations of sexual misconduct. “I can’t think of many (or any) participants in PBI Education courses or other remedial programs who were ordered to use a chaperone while they were under investigation,” she said.
Instead, regulators tend to use chaperones during a probationary period, that is, only after they have evaluated the evidence and concluded that the clinician can be safely returned to practice on a provisional basis. This determination is not made lightly. In fact, regulators demand convincing evidence that providers have learned the right lessons from their experience before granting them probation. In such cases, chaperones are assigned not to defend patients against suspected predators, but to keep an eye on well-intentioned clinicians while they work to justify the regulator’s faith in them.
Chaperones help support clinicians and patients.
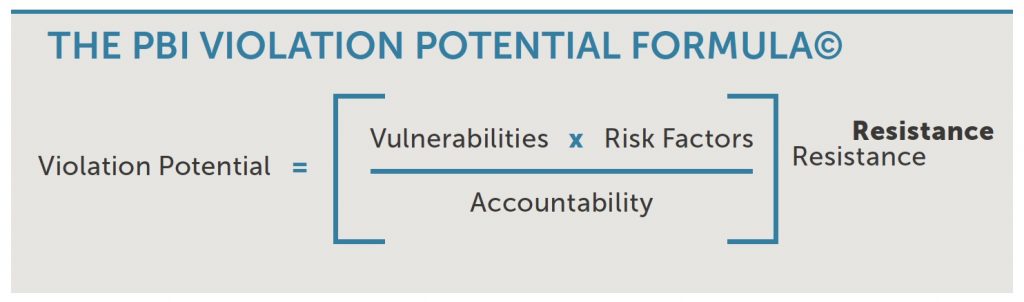
Social scientists tell us that accountability, knowing that we may have to justify our actions to a third party, leads us to think more seriously about the decisions we make and to make more responsible choices. That’s why Accountability functions as a moderating factor in PBI’s Violation Potential Formula.© As the Formula makes clear, external Risk Factors and internal Vulnerabilities increase a practitioner’s Violation Potential (VP). Resistance to confronting these challenges raises it exponentially. But bolstering Accountability will reduce one’s VP.
As objective third parties who are watching and listening, chaperones enhance physicians’ accountability. By doing so, they boost providers’ efforts to stick with their good intentions. That’s why many PBI graduates elect to use chaperones when they return to practice, even after the chaperone mandate has expired.
Chaperones provide other kinds of support as well, both to the physician and to the patient. A good chaperone can call a doctor’s attention to a patient’s unspoken concerns or help a reluctant patient ask questions that are troubling them. And just as the chaperone can help strengthen a well-intentioned doctor’s resolve, their presence can also help ease a patient’s concerns. In fact, that is the primary reason so many professional groups recommend having a chaperone available for intimate exams.
The chaperone’s ability to reduce tensions and misunderstandings protects patients from undue anxiety and physicians from unjustified charges of impropriety. And in those rare cases when patients do file charges, the chaperone serves as a valuable objective witness to what actually happened.
Chaperones are only as good as their training.
Given the vital role chaperones play, you would think chaperone training would be commonplace. It is not. At the time of this writing, very few formal training programs are available in North America.
To help remedy this situation, PBI Education has launched an online training program for anyone who may be asked to serve as a chaperone. The course offers two editions, drawing a clear distinction between two types of chaperones.
First, there are voluntary, as-needed chaperones, whose presence is requested (by patient and/or clinician) or is required per institutional policy or state law for all patients or all examinations of a certain type. Second, there are mandated chaperones, who are required by regulatory order or institutional mandate for a specific provider during certain patient interactions. As you would expect, the latter are held to a higher level of accountability. If a patient asks to speak privately with a doctor, a voluntary chaperone should step out of the room. A mandatory chaperone may not. If a patient is having trouble dressing themselves, an as-needed chaperone can offer to help. A mandated chaperone must not.
While noting the differences between the two types of chaperones, the course covers information vital to both. A combination of text, anatomical diagrams, links to additional material, and clinical vignettes helps students learn what to expect during encounters between physicians and patients. Physical exams in 10 different specialties, ranging from Cardio-Pulmonary to Urology, are explained, as are issues involving telemedicine and vulnerable patients.
The emphasis throughout is on the real world of chaperoning. With the help of videos and interactive scenarios, participants discover how easily everyday events can shift into reportable incidents, how to report and document what they witness, and how to handle challenging situations.
After taking the course, students are prepared for a wide range of clinical situations and professional challenges. They learn what to do and what not to do if a patient doesn’t want a chaperone in the room or if the patient is someone they know outside the office. They learn how to explain their role to other staff, how to protect themselves from harassment, even how to cope with ambiguous situations, when they aren’t sure if something is or is not a problem.
As the Australian report made clear, there are limitations to what chaperones can accomplish. But when properly trained and prepared, those who serve as chaperones provide a crucial and valuable support to doctors and patients alike.
More about the Medical Chaperone Training Program.
Developed upon request from numerous state medical boards, PBI’s Medical Chaperone Training Program launched in January 2020. The course is accredited by the California Board of Registered Nursing for 2 CE Contact Hours. Please contact our staff at 904-800-1237 with any questions about this course or others.
