Can Empathy be learned?
Can Empathy be learned?
Not all that long ago, empathy was thought to be “unteachable.” But a 2014 review of more than a thousand research studies concludes that “empathy can be enhanced through a variety of intervention types targeted toward medical students, residents, fellows and physicians.” The authors also conclude that the increases in empathy seem to last.
But while virtually everyone in medicine now believes that empathy is teachable, there is still a great deal of debate about how to get the job done. Courses focusing on communication skills are increasingly common (doctors’ empathy is pointless if they don’t communicate it to the patient) and several medical schools are turning to the humanities in an attempt to humanize their curricula. Weill Cornell Medical College, for example, has a Humanities and Medicine program that brings artists and writers to campus to speak to students.
Efforts begin even before students are accepted to medical school. The Association of American Medical Colleges (AAMC) has added a new section to the MCAT, the admission test for medical school, that seeks to factor in students’ understanding and capacity for empathy. In addition, notes an article in Greater Good, a publication of the University of California, Berkeley, AAMC is also “looking at other ways to assess applicants’ readiness for entering a career in medicine. These include using trained interviewers or standardized tests that measure applicants’ reactions to different doctor-patient scenarios, as well as allowing schools to assess applicants on more personal qualities, such as how they make decisions, handle stress, and respond when encountering patients from different backgrounds.”
NOTEWORTHY PROGRAMS. One group of physicians has been grappling with and learning about empathy for years. Psychiatrists devote much of their training to understanding the emotional complexities of patient-doctor interactions. They learn about transference (when a patient transfers feelings from past experience to the current situation) and counter-transference (when the therapist does the same thing in relating to a patient). According to forensic psychiatrist Funmilayo Rachal, “When we’re doing a good job with that, we can be very objective about what we’re experiencing and what the patient is experiencing, and also be aware of when we’re not doing a good job and be able to own that.”
But the educational experience in psychiatry—involving in-depth cases studies, close supervision and practical experience—is far more involved and intense than is practical in other fields of medicine.
Mindfulness offers another possible path for students. As suggested earlier, mindfulness can help doctors understand their own feelings, accept their limitations and engage emotionally with patients while maintaining a firm grip on their own reality. More than one medical school now includes mindfulness training in their curricula, and while the goals of programs at places like Georgetown and Brown Universities are not focused exclusively on empathy, one study of the Georgetown program showed that those who participated gained significant advantages in connecting with patients and others. Among the benefits: increases in positive emotions, concern for patients and an ability to handle negative interactions with others—all of which decreased empathy-restricting stress.
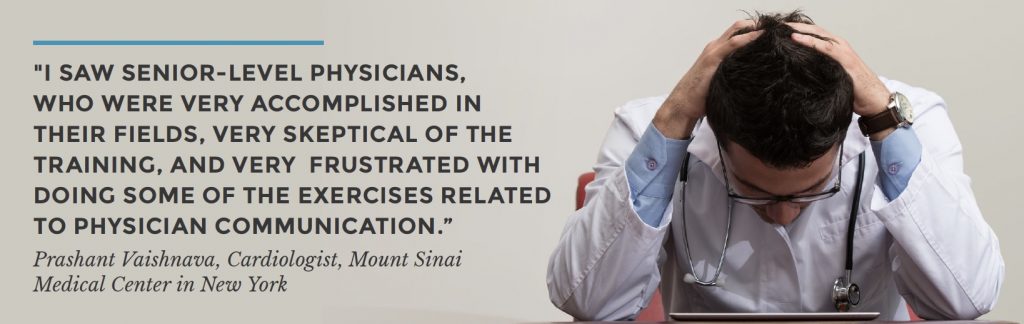
BEYOND MEDICAL SCHOOL. According to a recent Medscape article, experienced physicians, too, are enrolling in empathy training, either on their own or because they are being asked to do so. Cardiologist Prashant Vaishnava, assistant professor of medicine and director of quality assurance at Mount Sinai Medical Center in New York, reported that his hospital was rolling out a training program in empathic doctor/patient communication for physicians in a range of specialties. When the program was first offered, Vaishnava said, “I saw senior-level physicians, who were very accomplished in their fields, very skeptical of the training, and very frustrated with doing some of the exercises related to physician communication.” But eventually he saw even these experienced physicians “have these moments, these epiphanies, where they realized they could be doing better.”
Doctors in hospital-owned outpatient practices are also likely to receive empathy training, notes the same article, “not just to improve their quality of care, but also to protect market share. A hospital doesn’t want dissatisfied patients defecting to more empathic doctors in rival systems.” Even doctors in independent practices who score poorly patient surveys “are likely to be asked to improve their skills or risk deselection by health plans.”
One empathy-training program that appears to be gaining traction was developed by Dr. Helen Riess, a psychiatrist and medical educator at Massachusetts General Hospital and Harvard Medical School. Having established the program’s effectiveness, Reiss launched Empathetics, an independent for-profit company that offers both live and online training to physicians, nurses and other health care professionals.
The Empathetics protocol includes training sessions that focus first on the neurobiology of emotion. According to an article in the New York Times, “Doctors watch a video of a tense exam room interaction while a striking graphic sidebar records the electrical skin conductance of both patient and doctor, the mismatched spikes peaking as each person’s frustration with the other escalates.” Another session teaches clinicians how to recognize facial expressions—such as anger, contempt, happiness, fear, surprise, disgust or sadness—as well as other non-verbal emotional cues. The training also includes techniques for building emotional self-awareness and strategies for dealing with challenging patients, delivering bad clinical news, recognizing the impact of stress and fatigue on one’s own behavior and regulating personal stress responses.
