Who Is Disruptive and Why?
Who Is Disruptive and Why?
Understanding the causes of disruptive behavior helps explain why the problem persists.

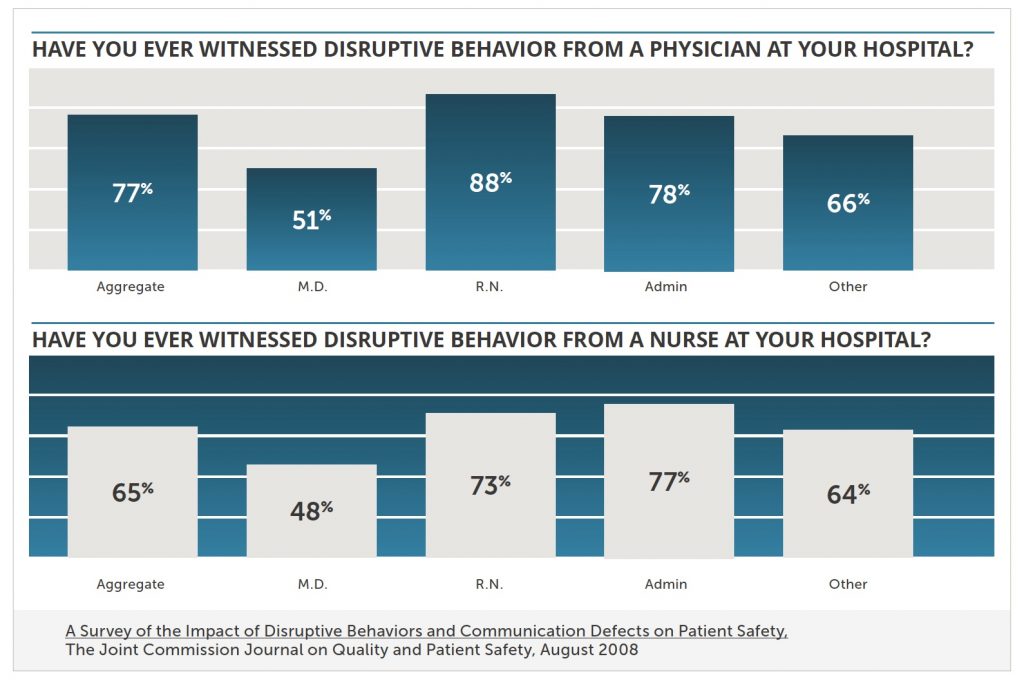
The problem is not simply a few arrogant physicians. Yes, physicians are the worst offenders when it comes to disruptive behavior, but nurses are not all that far behind. Overall, 77% of the respondents to the 2008 survey reported seeing physicians acting badly, while 65% witnessed such behavior among nurses. Of course, it depends on who is doing the counting. In general, physicians seem to be less sensitive to disruptive behavior than nurses. Fifty-one percent of physicians reported seeing their peers acting out, 48% reported the same problem among nurses. Nurses, however, saw disruptive behavior more frequently both among physicians (88%) and fellow nurses (73%).
Three overlapping causes. Regardless of who the offenders are, the causes of disruptive behavior fall into three broad categories.

The first is health care’s inherently stressful environment. Nurses, physicians, pharmacists and others have to manage their emotions, communicate clearly and work collaboratively, often under incredibly stressful conditions. Not only are the stakes high, but those involved are frequently overworked, exhausted and facing institutional pressures to increase productivity, contain costs and ensure satisfied “customers.” Many may also be contending with gender, cultural or age-related bias.
It’s hard enough for mature, well adjusted, emotionally resilient professionals to manage in this kind of stressful environment. For those with fewer inner resources, the challenge is far more daunting. Character traits that might be tolerated in less stressful situations—self-centeredness, defensiveness, aggression—can lead to explosive behavior when the pressure is on. Individuals without strong social, communication and coping skills can find themselves overwhelmed and lash out in desperation. Mental health problems, family issues and financial pressures make matters still worse.
Surprisingly, substance abuse is rarely a contributing factor. Fewer than 10% of disruptive physician behavior issues are related to substance abuse. What is almost always a root cause is institutional culture. Those predisposed to disruptive behavior might still avoid problems, despite the inherently stressful environment, if workplace culture actively supported them in their efforts—encouraging collaboration and team work, providing positive role models and consistently holding everyone to the same high standards. Unfortunately, that is rarely the case.
Starting in medical school, physicians are surrounded by supposed mentors and authority figures who are often openly disrespectful and verbally abusive to those lower in the institutional hierarchy. Students may be taught about professional etiquette in the classroom, but what they learn on the job is very different.
And once they start practicing, physicians, nurses and others continue to see disruptive behavior all around them. The “hidden curriculum” is clear: such behavior is not only tolerated but accepted as a routine part of institutional life. The lesson is reinforced when those with power, especially those who generate significant revenue, are given free rein.
A vicious cycle is often at work in these institutional cultures. According to a 2006 article in Patient Safety and Quality Healthcare, “Most hospitals have policies in place to address only the most egregious behaviors and often ignore patterns of disruptive behavior until they reach dangerous levels.” Generally, say the authors, disruptive professionals are simply advised to mend their ways in perfunctory counseling sessions. The only other response, reserved for those rare instances when the offense is deemed sufficiently serious, is outright termination. The article calls this the fly swatter/sledgehammer approach.
This either-or strategy discourages people from reporting incidents. Those who believe nothing will come of their complaint remain silent rather than risk retaliation. Those who believe their complaint will end a career, hold their tongue far too long, often until the situation becomes truly intolerable.
In the absence of reports, administrators see no reason to make changes. They continue swatting flies until a particularly outrageous event draws their attention. Then they reach for the sledgehammer.
And so the cycle continues. Comparing the results of its 2003 and 2013 surveys, the ISMP concluded, “Despite more than a decade of emphasis on safety, little improvement has been made. Widespread disrespectful behaviors in healthcare persist unchecked and are found at all levels of the organization and among all disciplines of staff.”
