Nine Ways to Improve Reporting:
Nine Ways to Improve Reporting:
What employers, regulators and others can do to encourage reporting
- The first TAKE REPORTS SERIOUSLY. It’s hard enough for physicians to report a colleague’s misconduct. Hospitals and practices that fail to respond make it that much more difficult. Employers can encourage responsible reporting by taking all reports seriously, and holding everyone—including high-profile clinicians and researchers—to the same high standards.
- LEAD BY EXAMPLE. According to the Federation State Medical Boards‘ (FSMB) 2016 Position Statement on Duty to Report, “FSMB has heard complaints from its member boards that hospitals and health organizations regularly ignore reporting requirements, find ways to circumvent them, or provide reports that are too brief and general to equip the board with relevant information for carrying out its regulatory functions.” If hospitals want physicians and other healthcare professionals to live up to their reporting obligations, the institutions must do the same.
- MINIMIZE THE HURDLES. “In a complex and bureaucratic health care system, with multiple layers of oversight, regulation and accountability, it is often difficult for individuals to know with whom they should be sharing information, or what steps are required of them,” notes the FSMB position statement. While this is particularly true for patients and their families, many professionals make the same complaint. Simplifying hospital policies and procedures as much as possible, and communicating them to everyone, removes an important obstacle.
- INCREASE EDUCATION. The Federation suggests that healthcare professionals be taught the importance of sharing information and the role they need to play in helping protect patients from misconduct. “Early education of medical students and residents is especially important in helping to change attitudes about reporting,” noted the FSMB position statement.
- MANDATE TRAINING. In most states, physicians cannot be licensed without proof that they have been properly trained to recognize and report suspected child abuse. No such requirement exists when it comes to reporting misconduct. One way to ensure that physicians understand their duty to report would be to require such training as a condition of licensure.
- SHIFT THE PARADIGM. “If reporting is always viewed as a punitive exercise, few will share information,” notes the Federation statement. Caldicott suggests physician think of reporting not as policing one another, but in terms of healing. “Physicians are skilled observers and they are healers,” she said. “By keeping our eyes and ears open for clues that our colleagues may be at risk of committing a violation, we can put those skills to good use.” The word remediation, she adds, means ‘to heal again.’”
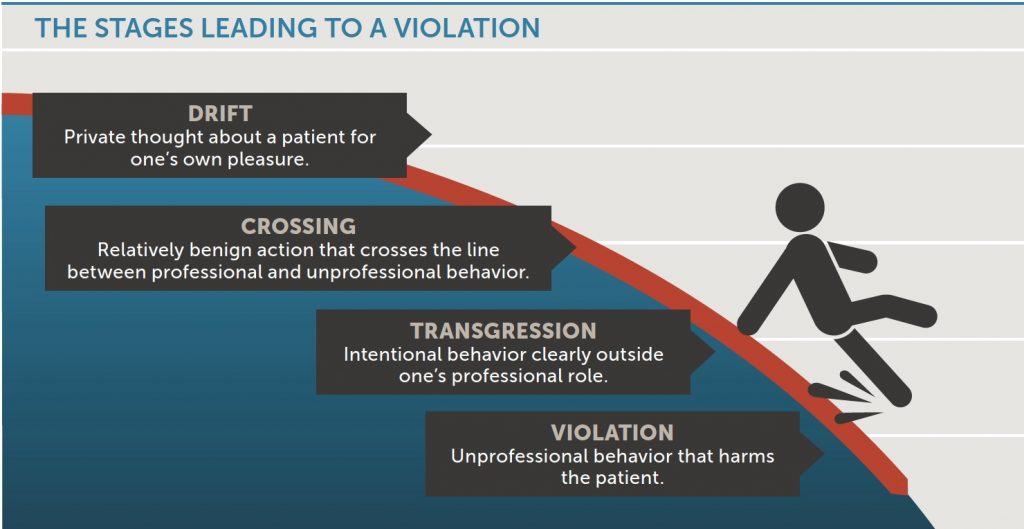
7. EMPHASIZE EARLY INTERVENTION. The importance of reporting egregious misconduct cannot be overstated. But focusing exclusively on extreme cases ignores the value of early intervention. Boundary violations are not isolated or random events. They are the final stage of a process that often starts with purely private thoughts (“drifts”) and proceeds through increasingly serious line-crossings. A practitioner might start out indulging in a harmless fantasy about a patient, then go on to schedule a follow-up sooner than clinically indicated. Eventually, the physician might ask the patient for a date and end up in a romantic relationship that is a clear boundary violation.
8. ENSURE CONFIDENTIALITY. Since one of the common reasons for not reporting is a fear of reprisal, it is important to ensure that those who do report misconduct have the right to confidentiality. It’s just as important to make sure everyone knows that right exists. Gaedeke now makes a point of telling physicians in Michigan that they are legally obligated to report misconduct and that their names will not be released without their written consent. By following her lead, hospitals and others can remove a serious barrier to timely reporting.
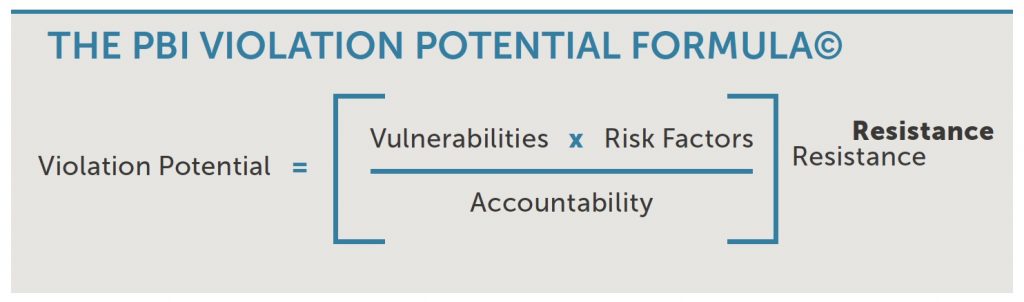
9. INCREASE ACCOUNTABILITY. In the PBI Violation Potential Formula (below), accountability acts as counterweight to the other forces people struggle with (individual vulnerabilities, risk factors and resistance). The more accountable someone feels, the less likely they are to commit a violation.
The same holds true for the duty to report. The more someone believes they will be held accountable for failing in their duty, the less likely they are to remain silent. And yet, those who neglect their legal and ethical obligations to report almost never suffer any consequences.
According to Caldicott, people are often referred to PBI Education and other similar organizations for failing to tell their boards about an arrest or loss of privileges. “That’s a violation of their state Medical Practice Act, and they get disciplined for it,” she says. “Yet I have never seen a physician disciplined for failing to report suspected sexual misconduct.” In fact, when someone asked if anyone at the FSMB meeting knew of someone being disciplined for failing to report, only one person, Anita Steinbergh of the State Medical Board of Ohio, responded.
There are a number of reasons discipline is rare. Some-times the law is unclear and, in many situations, evidence can be hard to come by. In the Ohio case, the Board learned that the junior partner in a pain management practice knew a senior colleague had been abusing female patients for years. The law in Ohio, said Steinbergh, is explicit: “You only have to have a reasonable belief that something is occurring and you must report,” she said. According to Ohio licensure defense attorney Beth Collis, the law “does not require absolute certainty or complete unquestioning acceptance, but only an opinion that a violation has occurred based upon firsthand knowledge or reliable information.”
Steinbergh made it clear that the Ohio Board had convincing evidence, including solid documentation, that the doctor in question knew what was going on and yet remained silent. After the senior partner voluntarily surrendered his license, the junior partner was brought to a hearing, said Steinbergh, and his license was permanently revoked. “That probably has not been done before,” she noted, “but we were certain that was the right action.”
View Other Posts
- Summer School: Reduce Stressors, Avoid Burnout
- Don’t Wait Until it is Too Late: How a Personalized Protection Plan© Decreases Violation Potential
- The What, Why, When, and How of Remedial Educational Interventions
- Revisiting Moral Courage as an Educational Objective
- If It Isn’t Documented, It Didn’t Happen
