How Effective is Regulator Oversight of Physicians?
How Effective is Regulator Oversight of Physicians?
Using FSMB data to compare the effectiveness of regulator discipline.
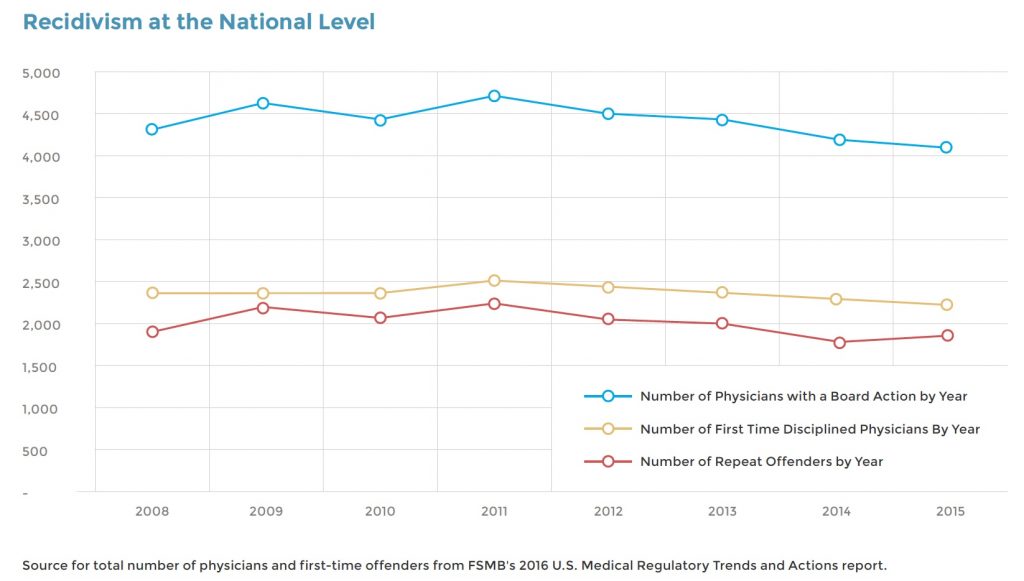
According to the Federation of State Medical Boards (FSMB), an average of 4,408 physicians were disciplined annually in the United States between 2008 and 2015. That number has remained remarkably steady, never varying from the average by more than 7%, despite a modest increase in the number of doctors during the period.
The FSMB itself draws no conclusions about these statistics, but others do. Public Citizen, a consumer advocacy group, has used Federation data to rank state medical boards for more than 20 years. The group’s methodology is simple: it compares the number of serious disciplinary actions (license revocations, surrenders, suspensions and probation/restrictions) to the number of doctors in each state. In its 2012 report, based on FSMB data, Public Citizen reported there were 3.06 serious actions per 1,000 physicians, an 18% decline from the peak rate of 3.72 per 1,000 physicians in 2004.
Assuming that the more disciplinary actions a board takes, the better, the report ranks state medical boards from “best” to “worst.” The best are those with the highest number of serious disciplinary actions relative to physician population; the worst are those with the least.
Some question the validity of this approach. “Public Citizen has it all wrong,” declared a 2010 Medscape article.
“Boards should not be judged by the number of licenses suspended or revoked, but by how well they protect the citizens of their state. Its simplistic analysis is akin to judging a city’s police department on the basis of the number of prisoners in its jails rather than the number of crimes committed. Most citizens are far more eager to live in a place with a low crime rate than with a high prison population.”
Public Citizen says that its report “does not purport to assess the overall quality of medical care in a state or to assess the function of the boards in other respects.” But it clearly assumes that the volume of serious actions is a fair measure of board performance, and local media have often used the report data to assail state boards and demand more aggressive actions against physicians. And the greater the outcry against boards that are “soft” on physicians, the more pressure there is on boards to take action.
Another Public Citizen study took a more sophisticated approach. Sydney M. Wolfe founded Public Citizen’s Health Research Group in 1971 and has co-authored many of the groups reports since then. In a 2016 study, Wolfe and colleagues from Public Citizen went beyond a simple ranking of serious actions to look at how boards responded to cases involving sexual misconduct. While noting, as others have, that medical boards discipline these violations more severely than other infractions, the study, which was funded by Public Citizen, faults the regulatory community for failing to adequately discipline physicians found guilty of sexual misconduct by the hospitals that employed them or in malpractice suits.
Using the National Practitioner Data Bank (NPDB), which collects the relevant data from hospitals and civil courts, the researchers found that between 2003 and 2013, 1,039 physicians were reported for sexual misconduct. Although the NPDB makes its data available to boards nationwide, state medical boards failed to discipline more than two-thirds of these doctors, according to the study. (Another Public Citizen study in 2011 reached a similar conclusion.)
It’s easy to exaggerate the significance of the study’s findings. As the authors themselves note, “Over the 10-year period of our study, only a small number of physicians were reported to the NPDB due to sexual misconduct.” In fact, the total number of cases considered averages just 104 annually, which means boards failed to act in 70 cases (two-thirds) each year. That also happens to be the number of state medical boards (the District of Columbia and U.S. territories each have a board). So on average, each board failed to act on a single case in a given year. (Some boards undoubtedly had more cases, while others had none at all, but the report does not provide state-by-state detail.)
But it’s also important to note that many sexual misconduct cases go unreported. The researchers mention several reasons why patients and colleagues often fail to file complaints, and a 2016 investigation by the Atlanta Journal-Constitution found that hospitals, too, sometimes withhold information. Private settlement agreements between doctors and hospitals are part of the problem, as are “legal loopholes and outright flouting of the law,” notes the article, “Dangerous Doctors, Flawed Data.”
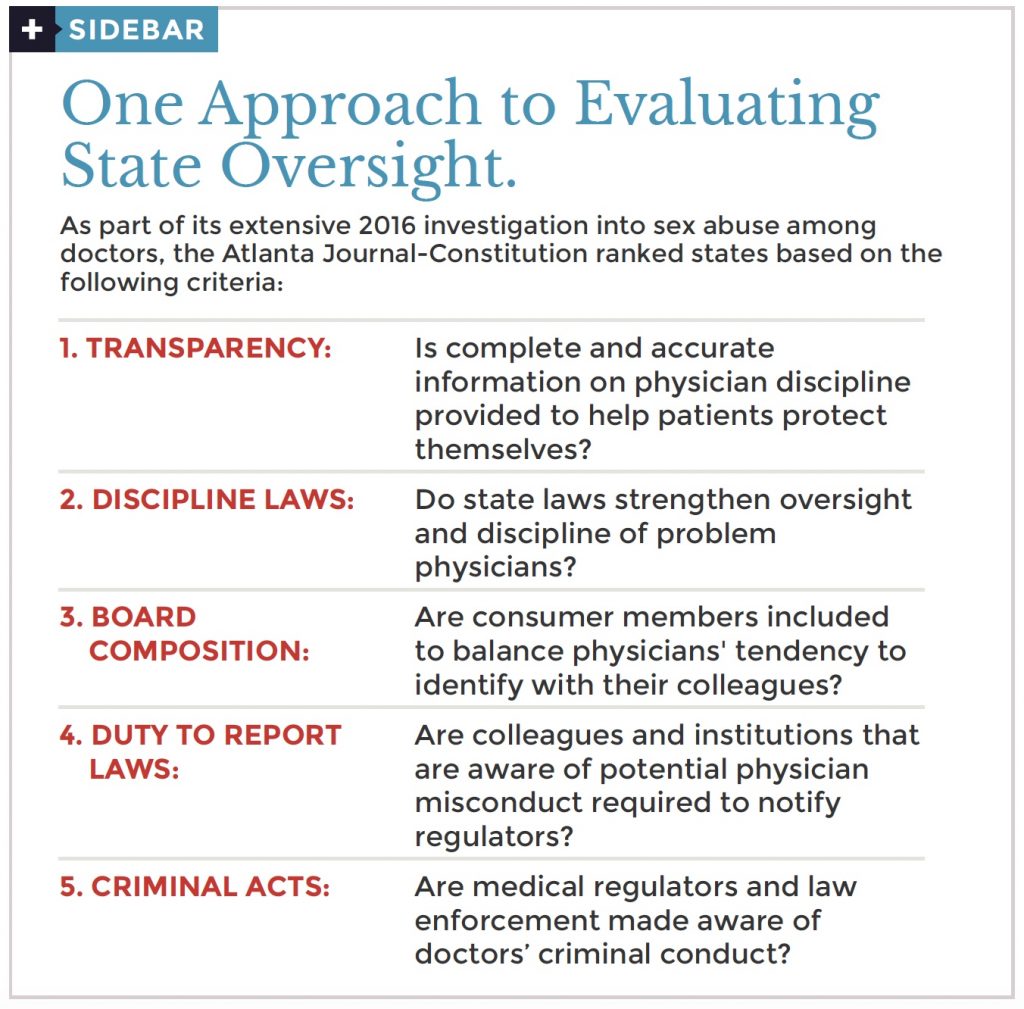
Other reports have used different criteria to evaluate physician discipline. A 2016 Consumer Reports article, “Can You Rely on Your State Medical Board,” focused on board websites. The state-by-state analysis looked at “how complete their information was and how easy the websites were to use.” The composite score for each state is thus a measure of the board’s transparency. The rating provides important information for patients who want to check out their doctor. It is less useful as a tool for evaluating board performance overall.
The Atlanta Journal-Constitution made transparency one of five categories it used to rate states. The others were Discipline Laws, Board Composition, Duty to Report Laws and Criminal Acts (see sidebar for more detail). But again, while providing useful information, the ranking does not actually measure individual board performance.
What is perhaps most significant in all these efforts is not what they report, but what they don’t. None of the investigations to date has looked at outcomes. In fact, according to several experts in the field, nothing has been written that relates board actions—or inaction—to patient wellbeing or public safety.
“I have never found, and would love to see, any sort of scientific evaluation of whether being more punitive or taking more disciplinary action leads to better patient outcomes,” says Jon Porter, a health care attorney who has both prosecuted and defended physicians over the past 20 years. “There is no data behind the assumption that the more discipline, the better the board,” he explains. ‘It doesn’t mean they’re better, just more punitive.”
One measure of effectiveness seems obvious: recidivism. How many physicians who are disciplined by boards go on to repeat their offense or commit even more egregious infractions? Surprisingly, few if any boards track recidivism, although experts report that most do deal more harshly with repeat offenders.
Research on recidivism is rare. A single study from 2007, “Sanctions and Recidivism: An Evaluation of Physician Discipline by State Medical Boards,” reviewed nationwide data for the period 1994 – 2002, and concluded, “There are a very large number of repeat offenders among physicians who have received board sanctions.” National statistics
can also be gleaned from FSMB’s “U.S. Medical Regulatory Trends and Actions” report. Although the report says nothing directly about recidivism, it does include data about both the total number of physicians disciplined each year and the number who are first-time offenders. The difference between the two, presumably the number of repeat offenders, suggests that a slight majority of those disciplined are recidivists.
What is remarkable about all three metrics is how stable they are. Despite the economic crash in 2008 and the subsequent recovery and despite the rapid rise in opioid deaths during the period, the total number of offenders and the number of repeat offenders barely changed over the eight years. Recidivism, at least at the national level, seems to be neither increasing nor declining.
But the FSMB data still doesn’t tell us anything about how individual boards are performing. That task, as virtually all the studies conclude, remains ripe for serious research.
View Other Posts
- Summer School: Reduce Stressors, Avoid Burnout
- Don’t Wait Until it is Too Late: How a Personalized Protection Plan© Decreases Violation Potential
- The What, Why, When, and How of Remedial Educational Interventions
- Revisiting Moral Courage as an Educational Objective
- If It Isn’t Documented, It Didn’t Happen
